Women’s Health

Modern hormonal contraceptives empowering family planning and sexual health
Thanks to modern hormonal contraceptives, couples today can better plan their families and enjoy sexuality with the confidence that pregnancy is preventable. The ability to make conscious decisions about whether and when to have children has significantly strengthened women’s roles in society. These contraceptives offer high reliability in preventing unplanned pregnancies and are reversible, allowing women to conceive after discontinuation1,2.
Diverse methods for individual needs
Hormonal contraceptives mimic the effects of the sex steroids estrogen and progesterone naturally produced by a woman's body3. Available forms include oral contraceptives ("the pill"), intrauterine systems (IUS), patches, vaginal rings, implants, and injectables4.
Personalized prescriptions
All forms of hormonal contraceptives require individual prescriptions, usually from a gynecologist. When selecting a method, factors such as a woman's age, medical history, current life situation, personal preferences, and expectations of the contraceptive should be considered5.
Bayer’s contraceptive options
Bayer offers a variety of contraceptive methods. It is crucial for doctors and patients to discuss all available options to ensure the patient receives the method best suited to her needs.
Patient advice
Each body responds differently to medications. It is essential to consult with your physician to determine the most suitable contraceptive for you.
References
|
Gynecological diseases like endometriosis can affect a woman's health, daily life, and overall well-being. They can also lead to high medical costs and impact the healthcare system.1
What is endometriosis?
Endometriosis is a long-term condition that affects women. It happens when tissue similar to the lining of the uterus grows outside the uterus. This tissue, called the endometrial tissue, behaves like the uterine lining—it thickens and breaks down during the menstrual cycle—but since it has no way to leave the body, it gets trapped. This can cause pain, swelling, and inflammation in the affected area.2
What are the causes of endometriosis?
The exact cause of endometriosis is unknown. There are different theories, but none have been fully proven. One common theory is retrograde menstruation, where menstrual blood flows backward through the fallopian tubes into the pelvic1 area instead of leaving the body. This tissue then attaches to different areas in the pelvic cavity and grows. However, not all women with retrograde menstruation develop endometriosis, so other factors may also play a role.3
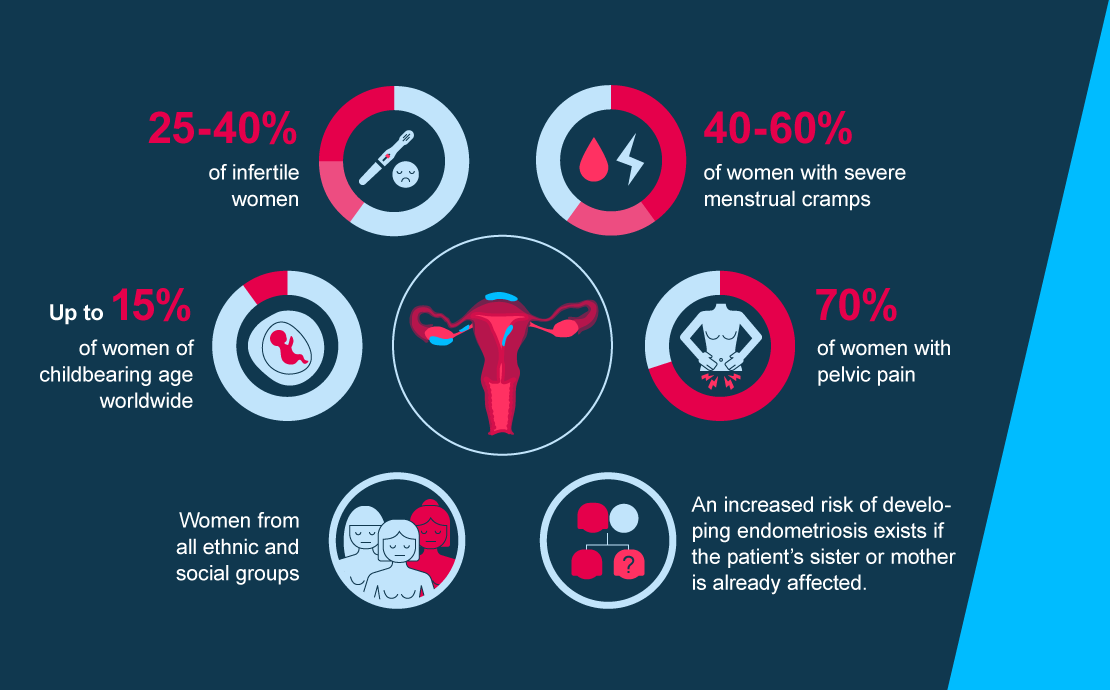
Who is affected by endometriosis?
Endometriosis primarily affects women of reproductive age.2
What are the symptoms?
The symptoms of endometriosis can be different for each woman. Common signs include dysmenorrhea (painful periods), noncyclic pelvic pain, dyspareunia (painful intercourse), dysuria (painful urination), dyschesia (painful bowel movements), fatigue, and subfertility (difficulty getting pregnant).4
Endometriosis is often diagnosed late, with delays of 6-10 years being common.5 This can cause ongoing physical pain and emotional stress, making daily life difficult. It can affect a woman’s studies, work, and overall well-being. Managing the condition often requires expensive medical and surgical treatments, leading to financial strain on both individuals and the healthcare system.1
Since 2010, Bayer has been offering a treatment specifically developed for endometriosis in Europe, several countries in Latin America, and Asia Pacific. It’s important for doctors and patients to discuss all treatment options available to make sure the patient receives the best medicine for her needs.
Advice for patients
Each patient’s body responds differently to medications, so it's hard to say which medicine will work best for you. It's important to speak with your doctor to find the treatment that’s right for you.
References
|
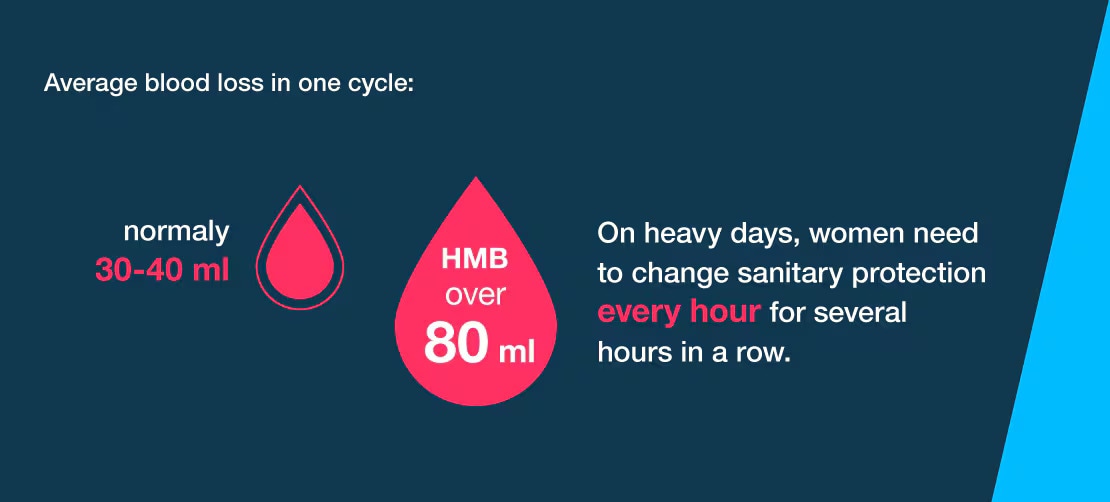
Many women don't realize that heavy menstrual bleeding (HMB) is a medical condition that can affect their quality of life.
What is heavy menstrual bleeding?
Heavy Menstrual Bleeding (HMB) is a condition where excessive bleeding during periods affects a woman’s daily life. It can happen on its own or along with other symptoms.
On average, 1 in 3 women will experience Heavy Menstrual Bleeding (HMB) at some point in their life1. For most women, the cause of HMB cannot be identified2.
Despite how common and impactful it is, many women don’t know that Heavy Menstrual Bleeding (HMB) is a medical condition. Almost 59% of women with HMB think it’s just a normal part of having a period3. It can be hard for women to know what counts as a heavy period, as menstruation varies from one woman to another.
What are the symptoms?
Symptoms of HMB include:
• Heavy and prolonged menstrual periods4
• Symptoms of anemia such as tiredness, fatigue, shortness of breath5
• Lower abdominal and pelvic pain6
There are various contraceptive methods approved for treating Heavy Menstrual Bleeding (HMB), including products from Bayer7. It’s important for doctors and patients to discuss all available treatment options to ensure the patient gets the best medication for her needs.
Advice for patients
Everybody responds differently to medications, so it’s not possible to know which medicine will work best for you. It’s important to consult your doctor to find the right treatment for you.
References
|





